Everything You Need to Know About the HPV Vaccine
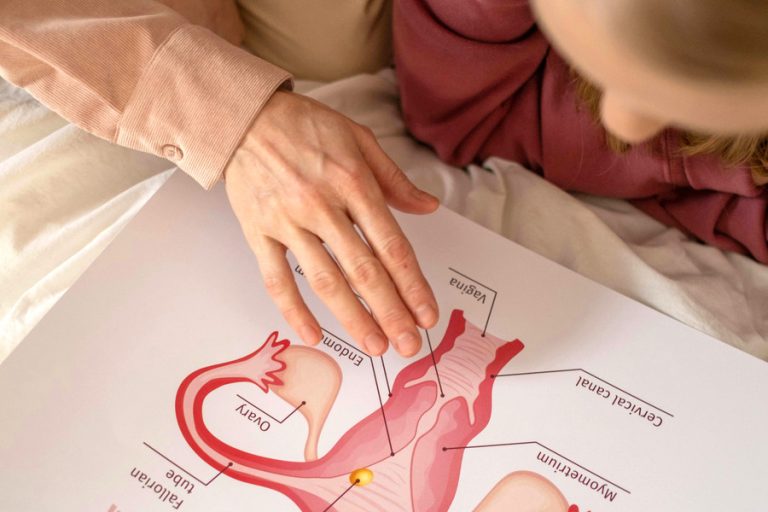
Human Papillomavirus (HPV) is one of the most common sexually transmitted infections (STIs) in the world, affecting millions of people each year. Although many HPV infections resolve on their own without causing serious problems, some strains can lead to severe health conditions, including cervical cancer, other genital cancers, and throat cancers. The good news is that there’s a powerful tool to prevent these outcomes—the HPV vaccine.
In this blog post, we’ll take a deep dive into what HPV is, how the vaccine works, who should get it, and why it matters.
What Is HPV?
HPV refers to a group of more than 200 related viruses. About 40 of these can be spread through direct sexual contact and infect the genital area, mouth, or throat.
Most HPV infections are asymptomatic and go away on their own. However, some types (notably HPV-16 and HPV-18) are known as “high-risk” strains and are responsible for:
-
Over 90% of cervical cancer cases
-
Majority of anal, penile, vulvar, and vaginal cancers
-
A significant number of throat (oropharyngeal) cancers
Other “low-risk” types can cause genital warts and respiratory papillomatosis, a condition where benign tumors grow in the air passages.
What Is the HPV Vaccine?
The HPV vaccine is a safe and effective immunization designed to protect against the most harmful types of the virus. The most widely used HPV vaccine today is Gardasil 9, which protects against nine HPV types—seven high-risk types and two low-risk types that cause genital warts.
How Does It Work?
The vaccine works by stimulating the immune system to produce antibodies against HPV. This preparation helps the body recognize and fight the virus if exposed later. Importantly, the vaccine does not contain live virus and cannot cause HPV infection.
Who Should Get the HPV Vaccine?
Age Recommendations:
-
Children and Teens (Ages 9–14): The CDC recommends vaccination starting at age 11 or 12, but it can begin as early as age 9. Two doses are typically sufficient.
-
Older Teens and Young Adults (Ages 15–26): A three-dose schedule is recommended.
-
Adults (Ages 27–45): Vaccination in this group is based on individual risk and should be discussed with a healthcare provider. While not routinely recommended, it can still provide benefits, especially for those who haven’t been exposed to all HPV types.
Why Vaccinate Early?
The vaccine is most effective when given before exposure to HPV, which is why it’s ideally administered before individuals become sexually active. However, even those who are already sexually active may benefit.
Is the Vaccine Safe?
Yes. The HPV vaccine has been rigorously tested and monitored for safety. More than 15 years of data from millions of people show that it is very safe and highly effective. Like all vaccines, it may cause mild side effects such as:
-
Pain or swelling at the injection site
-
Mild fever
-
Headache or fatigue
Severe allergic reactions are extremely rare.
What Are the Benefits?
1. Cancer Prevention
The most significant benefit of the HPV vaccine is its role in preventing cervical and other cancers. Studies have shown a dramatic decrease in HPV infections and cervical precancers in vaccinated populations.
2. Reduction in Genital Warts
The vaccine also prevents HPV types that cause about 90% of genital warts, leading to a visible improvement in public health outcomes.
3. Herd Immunity
Widespread vaccination can reduce the overall presence of HPV in the population, offering protection even to those who are unvaccinated.
Common Myths and Misconceptions
Myth 1: The HPV vaccine encourages sexual activity.
Fact: Studies consistently show no increase in sexual activity or earlier onset of sexual behavior in vaccinated adolescents.
Myth 2: Only girls need the vaccine.
Fact: HPV affects everyone. Vaccinating boys is just as important—it protects them and helps prevent the spread of the virus.
Myth 3: It’s too late to get the vaccine if you’re already sexually active.
Fact: You may still benefit, as it’s unlikely you’ve been exposed to all nine types covered by the vaccine.
The Global Impact
Countries with high HPV vaccination rates—such as Australia, the UK, and Rwanda—are seeing incredible results, including reduced rates of cervical abnormalities and predictions of cervical cancer elimination within decades.
Final Thoughts
The HPV vaccine is a modern medical success story. It’s safe, effective, and one of the most powerful tools we have to prevent cancer. Whether you’re a parent making decisions for your child, a young adult considering vaccination, or someone catching up later in life, the choice to vaccinate can have lifelong health benefits.
If you haven’t already, talk to your healthcare provider about the HPV vaccine—it’s a small step that could make a huge difference.
Protect yourself. Protect others. Prevent cancer. 💉